MALE CIRCUMCISION a paediatric surgical perspective
Dr Yogendra Kumar Punia and Mr Anthony Lander discuss paediatric indications for circumcision
Introduction
Circumcision has been practiced for religious reasons, for prophylaxis against perceived future ailments and for immediate medical indications which are discussed here. Perspectives on circumcision in the Muslem and Jewish communities appear elsewhere in this issue. These and other perspectives with discussions on legal issues, children’s rights and the effects on sexual function have been recently extensively reviewed (4). Preputial natural history The prepuce and glans of the penis have a common epithelium, which gradually separates, and keratinizes. This process is completed anytime from late gestation to the teenage years. The common epithelium is often termed “preputial adhesions” an unfortunate term implying pathology. This normal anatomy prevents full retraction in up to 60% of children till 6-9 years of age but usually disappears by 17 years (2).
Preputial symptoms and pathology

True phimosis: an absolute indication for circumcision True phimosis (Figures 1) affects 1.5% of boys by the age of 17 (5) (2), and is rare before 5 years of age (6). It can be asymptomatic or present with irritation, dysuria, bleeding, acute and rarely chronic urinary retention and non-retractability. Sometimes the foreskin has previously been retractile. The epithelium is hyperkeratotic with lymphocytes present. Beneath the epithelium there is an oedematous hyalinized poorly cellular layer of collagen. This is called balanitis xerotica obliterans (BXO), and is similar to lichen sclerosis et atrophicus which is seen in girls. Its aetiology is unknown. Occasionally scarring follows trauma from forced retraction and looks similar to BXO.
Acute balanoposthitis
Acute balanoposthitis is inflammation of the glans and foreskin usually with a discharge from the preputial orifice. It may result from infection in the separating epithelia and in most boys it settles spontaneously in one or two days. Balanoposthitis is not an indication for circumcision, unless there are recurrent troublesome attacks. Oral or topical antibiotics have no demonstrated role.
Ballooning
Ballooning of the foreskin (rarely seen with true phimosis) is usually asymptomatic and does not damage the urinary tract. Sometimes the trapped urine leaks after micturition and can present as wetting. Gentle proximal traction on the foreskin during micturition resolves the problem of wetting. Lumps in the foreskin Infants are sometimes referred with a yellow/white discrete subcutaneous lump on the penis. This is usually trapped preputial smegma which will discharge itself as the foreskin separates from the glans.
Paraphimosis
In paraphimosis a retracted foreskin acts as a tight and apparently irreducible band proximal to the coronal sulcus and is complicated by increasing preputial and glandular oedema. Often it results when parents have been instructed to pull the skin back without advice on replacing the foreskin over the glans. It can usually be reduced with distal preputial traction but this is impossible if the glans is pushed proximally to try to pass it through the narrow foreskin. General anaesthesia may be necessary for reduction but circumcision is only rarely needed.
Examination of the foreskin to distinguish a normal from a pathological phimosis In newborns and infants the prepuce is usually non-retractile this is normal. Gentle attempts to retract the non-pathological, non-retractile foreskin demonstrate a narrow blanching preputial bottle neck (Figure 2 A) and the preputial orifice being soft and unscarred everts to demonstrate its distal inside epithelium. Pathological or true phimosis is recognised by pale, hard, fibrous tissue at the preputial orifice (Figure 1). This narrowing does not evert to demonstrate its distal inside surface (Figure 2 B).
Postoperative complications and management
Most medically indicated circumcisions are performed electively as day-cases, with general anesthesia and a penile or caudal nerve block. Complications are seen in a small number of boys only. A small amount of bleeding is common and < 1% of boys may require re-operation for bleeding or occasionally evacuation of haematoma. Superficial crusting is common and is not usually a problem but infection and septicaemia though rare can be serious. Crusting or meatitis can narrow the meatus causing spraying and dysuria, which usually resolves in 7-10 days. Rarely meatal stenosis or stricture may develop after some weeks perhaps in relation to ongoing BXO. A dilatation or meatotomy may be needed, hydrocortisone may help. Chloramphenicol ointment, petroleum jelly or lignocaine gel applied to the meatus and glans 3 or 4 times a day for 3 or 4 days may help reduce meatal stenosis, crusting and infection, and reduce adherence of the glans to adjacent underclothes. Simple analgesics like paracetamol are prescribed.
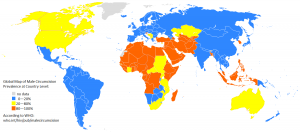
Routine neonatal circumcision: a controversy
Neonatal circumcision, widely practiced in the USA, has been advocated to reduce the incidence of penile and uterine cervical carcinoma and sexually transmitted diseases including HIV, but the evidence is equivocal and does not support mass involuntary circumcision. On the other hand, urinary tract infections though rare in male infants are more common in the uncircumcised boy. But about 100 neonates would need to be circumcised to reduce the risk of urinary tract infection in one boy. We do not therefore advocate neonatal circumcision. If it is carried out it is contraindicated in the premature, those who are ill or who have bleeding disorders or in the presence of congenital anomalies especially hypospadias.
Conclusion
Incomplete retraction of the prepuce is normal in neonates and infants with preputial separation from the glans progressing spontaneously until adolescence. (1-3). Asymptomatic non-retraction is not an indication for forced retraction nor circumcision, nor is it a predictor of future preputial problems. The commonest medical indications for circumcision are balanitis xerotica obliterans (BXO) and recurrent troublesome balanoposthitis check out daily cialis side effects.
Key points
* The asymptomatic non-retractile foreskin (“preputial adhesions”, “physiological phimosis”) usually becomes retractile spontaneously by adolescence and usually much sooner
* Circumcision is medically indicated for the 1.5% of boys (mostly over 5) who develop a true phimosis (Balanitis xerotica obliterans)
* Circumcision is medically indicated for a few boys with recurrent troublesome balanoposthitis
* No evidence supports a role for regular attempts to retract the non-retractile foreskin, either in the bath at home or under general or local anaesthesia
* No solid evidence justifies mass neonatal circumcision
